PRP stands for Platelet Rich Plasma. It is a form of orthobiologic treatment which is essentially using the body’s own natural healing components to speed up the healing process. PRP is acquired from the patient’s own blood through a process known as centrifuging.
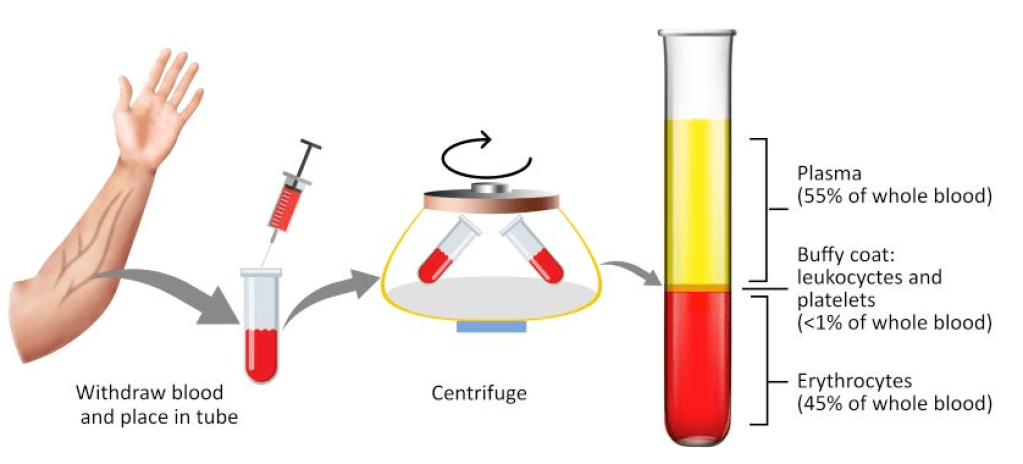
The patient’s blood is collected in a special container (30-60 ml, depending how much PRP needs to be extracted) that will be placed in a centrifuge. The container is then spun for a few minutes and the blood separates to 3 distinct component as seen in the image above. The PRP is the top portion of the buffy coat. 30 ml of PRP allows us to yield 3-5 ml of PRP. Concentration of platelets in PRP is 2.5 to 8 times normal blood levels (this depends on the kit used)
PRP is rich in proteins and growth factors that not only speed up the healing of tendons, ligaments, muscles and cartilage (tissue regeneration), it also has the ability to reduce excess inflammation and modulate pain.
- Platelet-derived growth factor (PDGF): A glycoprotein that activates cell membrane receptors and initiates activities like angiogenesis, mitogenesis, and macrophage activation.
- Transforming growth factor-β (TGF-β): Secreted by platelets and macrophages, TGF-β is involved in bone regeneration, long-term healing, and bone modeling.
- Vascular endothelial growth factor (VEGF): A signal protein that stimulates angiogenesis and vasculogenesis.
- Epidermal growth factor (EGF): A growth factor that stimulates cell growth, proliferation, and differentiation.
- Fibroblast growth factor (FGF): A growth factor in PRP
- Insulin-like growth factor (IGF): A growth factor in PRP that mediates growth and repair of skeletal muscle, chemotaxis, and bone formation
Since this product is obtained from patient’s own blood, the risk of allergic reactions are close to none.
The PRP is then injected to the site of desire (muscle, tendon, ligament or joint) usually under Ultrasound guidance to ensure accuracy of delivery. This is a completely outpatient treatment. No hospitalisation is required. After the procedure you may have some discomfort for 48-72 hours which is self limiting. Pain medication especially Non-steroidal anti inflammatory drugs like diclofenac, celecoxib and its close varieties, and ice therapy are not encouraged as it may slow down the healing process. The rehab protocol may vary but usually there is a 2 week downtime post treatment to allow the PRP to effectively assist the healing process. After 2 weeks there is a gradual return to exercise.
Indications of PRP injections includes muscle tears, tendon injuries – both acute and chronic, ligament injuries – both acute and chronic, and cartilage injuries. PRP is a go to option before exploring operative management in many musculoskeletal injuries.
- Tennis elbow
- Golfer’s elbow
- Grade 2 muscles tears
- Long head of biceps tendinopathy
- Rotator cuff injuries
- Early knee osteoarthritis – usually in combination with Hyaluronic Acid
- Partial ACL injuries
- And many more….
When is PRP not suitable?
PRP is not suitable in:
- Elderly individuals : Those above 60 have a tendency to have lower levels of platelets, blood levels of growth factors are lower and there has been evidence that there are higher levels of pro-inflammatory markers in the blood.
- Cancer: Any person with active cancer especially leukemia or bone cancers. – they directly impact the quality of PRP and it may affect the cancer progression.
- Blood disorders : Severe anemia, thrombocytopenia , Von Willebrand disease – poor levels of platelet and lower quality of platelets. Even those on prolonged NSAIDs and Aspirin may have poor quality platelets.
- Infections : Those in any active state of infection like sepsis
- Autoimmune disease : Those with any of these conditions, can be exacerbated by PRP injections. Conditions like serum sickness may happen.
- Cardiac conditions : Unstable angina
